All You Need to Know About Incontinence: Incontinence 101

Incontinence is more common than you might think. Over 25 million adults in America are managing temporary or chronic urinary incontinence. It is not easy to deal with or talk about, either. Many people avoid discussing it, even with their healthcare providers. They may find it embarrassing or think it is a normal part of life, even though it can be treated or managed.
Fortunately, there are many things you can do about incontinence, like exercises and wearing absorbent products. If you or a loved one has incontinence, learn more about the condition and incontinence treatment options.
What Is Incontinence?
Incontinence refers to the involuntary loss of urine or feces. It can be temporary or chronic, affecting people of all ages. Urinary incontinence is more common, but fecal incontinence is also prevalent:
-
Urinary incontinence: The urinary system typically works by tightening muscles in the bladder to move urine to the urethra. The muscles around the urethra then relax so urine can pass out of the body. When muscles in and surrounding the bladder are not working correctly, the urine can leak out when not intended. Some common causes of urinary incontinence include activities where downward pressure occurs, such as a sneeze or a cough.
-
Fecal incontinence: Fecal incontinence is the accidental loss of a bowel movement. Proper bowel functioning relies on muscles in the rectum and anus working correctly. The rectum needs to stretch to hold stool, and the sensation of "needing to go" must be sent to the brain. Anal sphincters must also work correctly to squeeze the anus shut and prevent the release of stool. If any of these structures do not work properly, the individual might experience fecal incontinence. Urinary incontinence often comes with fecal incontinence.
Both types of incontinence can have effects that reach far beyond bathroom problems. Some people avoid social outings for fear of leaks, and many feel isolated or embarrassed because of their situation. Unfortunately, it can contribute to psychological disorders like depression, anxiety and anger. These severe effects are part of why incontinence management is so critical. It is not something to be ashamed of. Understanding and managing the medical condition of incontinence can play a significant role in the psychological health of those who deal with it.
How Common Is Incontinence?
The prevalence of incontinence is much higher than many people think. Studies have found that 25%-45% of people will deal with urinary incontinence. In women over 70, more than 40% of the population is affected.
The rates are even higher in nursing homes, with 77% of women in nursing homes dealing with urinary incontinence and about 47% of all nursing home residents dealing with both urinary and fecal incontinence. Fecal incontinence is one of the top three reasons for admittance into a residential care facility.
Some factors that can affect the prevalence of incontinence include:
-
Age: Muscle strength tends to decrease as you get older, making older adults prime candidates for incontinence. Some people think that incontinence is a normal part of aging. While common, it is not inevitable, nor should it be left untreated.
-
Gender: Gender is also significant, with women being twice as likely as men to have incontinence. This is partially related to pregnancy, childbirth and menopause, which can cause incontinence issues by weakening the pelvic muscles. Of course, men can also experience incontinence, often due to enlarged prostates or prostate cancer.
-
Obesity: Obesity is also associated with an increased risk of urinary incontinence.
Despite how common incontinence is, many people feel isolated and ashamed. Yet, others do not even want to acknowledge it as a problem because they see it as a normal part of aging or having children — which it is not. Only 45% of women who experienced weekly urinary incontinence episodes brought it up with their healthcare providers.
This lack of open discussion can contribute to the effects of incontinence and cause it to be more of a burden to the individual. Not visiting a doctor can prevent someone from discovering treatment options or finding better incontinence management supplies. Know that incontinence is quite common and that a person with this issue is not alone. Dealing with incontinence can seem embarrassing, but it is nothing to be ashamed of. It is a medical issue that can be managed and does not need to impact anyone's ability to live life to the fullest.
What Types of Incontinence Are There?
Incontinence can come in many forms. In addition to urinary and fecal types, we can also categorize incontinence by how it occurs. Here are some different types of incontinence:
-
Stress: You might see stress incontinence when the pelvic floor muscles are weak and pressure is applied to them. Movements and certain activities can trigger it. Examples of stress incontinence would be releasing urine while sneezing, coughing, exercising or lifting heavy objects. It comes from a difficulty containing urine or stool in the body and is also called Stress Urinary Incontinence (SUI).
-
Urge: With urge incontinence, the individual might have a sudden, intense urge to use the bathroom but cannot reach it in time. People who have had a stroke or deal with conditions like diabetes, Parkinson's disease or Alzheimer's disease may find themselves having urge incontinence. It is also called overactive bladder (OAB) and affects more than 30% of men and 40% of women in the United States.
-
Overflow: If the bladder does not empty properly, it can overflow and leak urine from the body. It often presents as small amounts of urine leaking from a bladder that is not completely emptied during urination. Overflow incontinence might occur for someone who has trouble emptying their bladder due to issues like an enlarged prostate or spinal cord injury.
-
Functional: Functional incontinence occurs when another condition, such as arthritis, keeps the individual from reaching the bathroom in time. It typically comes from disorders that make it difficult to move quickly after the person feels the need to "go."
-
Mixed incontinence: Many people also experience more than one type of incontinence. This term often refers to experiencing stress and urge incontinence, but it can refer to other mixes
What Causes Incontinence?
Many factors can cause or contribute to incontinence, including lifestyle factors like diet and physical activity. Some causes might be harder to control, such as nerve disorders or other medical issues. Generally, incontinence is caused by muscle issues in the bladder, bowels or pelvic floor or nerve problems that affect the body's signals for needing to go to the bathroom.
Some causes of incontinence include:
-
Weakened or overactive muscles in the bladder, rectum, anus or pelvic floor.
-
Cognitive disorders, such as dementia and Alzheimer's disease.
-
Infections, including urinary tract infections or vaginal infections.
-
Constipation.
-
Pregnancy and childbirth.
-
Blockage from an enlarged prostate.
-
Conditions that make it hard to reach the bathroom in time, like arthritis.
-
Some medications, like drugs for high blood pressure, diuretics and sleeping pills.
-
Nerve issues, such as those from multiple sclerosis, diabetes, Alzheimer's disease, Parkinson's disease, spinal cord injuries or strokes.
Diet and Exercise
Diet and exercise can also play a role in incontinence. Many exercises focus on the specific muscles involved in incontinence, but general weight loss can also help. Additional weight can put more pressure on the bladder, and studies have found that losing just 5%-10% of body weight can help control urinary incontinence.
Many foods and drinks can also cause or contribute to incontinence. These substances typically irritate the bladder or act as diuretics, which increase urine production. Some bladder irritants include:
-
Alcohol
-
Caffeine
-
Chocolate
-
Artificial sweeteners
-
Spicy or acidic foods
-
Carbonated beverages
-
Tobacco from smoking
Some people adjust their diet by limiting or increasing their fluid intake. While there are many things you can do to improve bladder health, limiting fluid intake typically isn't one of them. Minimizing fluids might sound like it would make you urinate less, but it can cause more problems. Drinking less makes your urine highly concentrated, irritating the bladder and even encouraging bacteria growth. Increasing fluids can increase the need to urinate. Fluid intake requirements will vary for each person, so speak with a doctor before making any adjustments.
Can Incontinence Be Cured or Treated?
In some cases, incontinence can be cured entirely or significantly treated. Even if it cannot be cured, various management options make living with incontinence easier.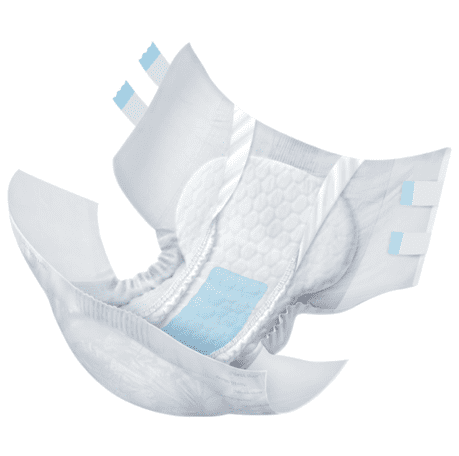
Absorbent Incontinence Supplies
Almost 60% of adults with incontinence use absorbent supplies to keep leaks in check. These products are discreet and can be worn underneath clothing to keep the wearer clean and dry without drawing attention to leaks. Absorbent products are specially designed for this purpose, with special materials that pull leakage away from the skin.
Absorbent incontinence supplies are available in many forms to fit different needs and preferences. Some styles include pull-on diapers, protective underwear and tab-style diaper briefs. Diapers with tabs are good for individuals with caregivers because they are easier to work with, while pull-on diapers are popular for people who want an experience similar to underwear. You can also find waterproof covers, liners and pads that lay on top of underwear and other absorbent supplies.
In addition to wearable products, absorbent bedding protection is available to help with overnight incontinence. Other useful supplies include wipes and disposable bags. These materials can help mitigate the effects of incontinence and allow people with the condition to enjoy life freely. They can stay dry and go about their day without worrying about embarrassment from incontinence.
Pelvic Muscle Exercises
Pelvic muscle exercises can strengthen bladder muscles for some types of incontinence, particularly stress incontinence. Also called Kegels, these exercises are best suited for stress incontinence, urinary urge incontinence and fecal incontinence. Many online sources explain how to do them, but a healthcare provider can also teach someone how to do pelvic muscle exercises.
Lifestyle Changes
Individuals can often mitigate certain types of incontinence with lifestyle changes to diet and exercise. Someone with incontinence might try to lose weight or avoid the foods we mentioned in the last section that can contribute to incontinence.
Bladder Training
Bladder training involves changing your bathroom habits and is usually used for stress or urge incontinence. It can help increase control over the bladder and extend how long someone goes between bathroom trips. Bladder training can include pelvic muscle exercises and delaying urination to improve your ability to hold it in after feeling the urge to go. Another part of bladder training might be scheduling bathroom trips and going at a specific time, whether or not the person needs to go. Talk with a doctor about bladder training before trying it.
Medication
Medications can reduce some kinds of leakage, namely overactive bladders and urge incontinence. They may help send the right signals to the brain or relax or strengthen specific muscles. Of course, medication can get complicated, so if you are considering it, have a conversation with a doctor to find the best one.
Surgery and Medical Devices
Finally, surgery and medical devices can help control or treat some types of incontinence. Incontinence caused by the position of the bladder or a blockage may be treated with surgery. Other surgeries can adjust the structures to support the urethra or bladder.
Medical devices can also be used, especially for stress incontinence. These include urethral inserts and pessaries. Urethral inserts are disposable devices used before activities that can trigger stress incontinence. They work like a plug to prevent leaks. A pessary is a device inserted into the vagina to support the urethra and is worn all day.
Incontinence Management With NorthShore
Incontinence can be stressful, but the right supplies can make managing it easier. Here at NorthShore, we offer assurance through dependable, protective absorbent products that offer up to three times the leak protection of leading store brands. We offer:
-
Adult diaper briefs: Adult diaper-style briefs offer excellent protection and are easy for another person to use, such as a caregiver.
-
Adult pull-on diapers and protective underwear: These two styles pull on over the legs just like typical underwear, but they offer absorbent support for leaks.
-
Liners and pads: Liners and pads can be used discreetly within the individual's underwear to offer lighter protection. They can also prevent leaks that can occur around leg openings.
-
Booster pads: Booster pads are used with another absorbent undergarment to increase protection, reduce the number of changes required or prevent leaks around leg openings.
All are available in many styles and sizes and shipped with discreet packaging. We also offer other incontinence supplies, like personal care products and bedding protection. However you or your loved one choose to deal with incontinence, we make products designed to help you live life worry-free.
Thank you so much for reading our blogs!
Did you know NorthShore has helped millions of people manage incontinence with life-changing absorbent products? It's so amazing to hear their stories.
We also want you to know we have trained product advocates that provide a personal experience by working with each customer to find the best product for their situation.
Find out for yourself today!
To get in touch, simply provide your contact details below and your personal product advocate will reach out.












